
This article was published on Arbona Health Hub Volume 1 Issue 1 (ISSN: 3065-5544).
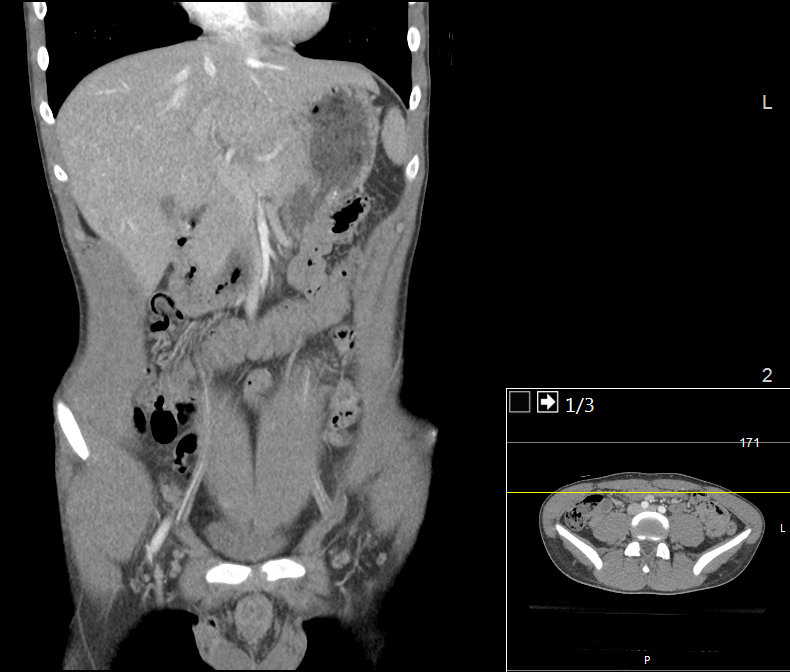
The Computer Tomography (CT) scan represents a widely used and valuable imaging diagnostic tool in modern medicine. It enables medical professionals to detect the presence of tumors, traumatic injuries, hemorrhages, and a range of other health abnormalities (Computed Tomography (CT), 2022).
Mechanism of CT Scans
The technique uses a rotating X-ray beam around the patient to generate cross-sectional images, which are then processed and subsequently stacked to create a 3D image. However, the procedure requires exposure to ionizing radiation, which poses a potential threat to DNA. Ionizing radiation can lead to single-stranded and double-stranded DNA breakages, which may lead to mutations and, ultimately, to cancer. Although the radiation doses used in CT scan procedures are considered generally safe, concerns have been raised regarding children, who are more susceptible to the harmful effects of ionizing radiation, as well as those patients who undergo repeated exposures.
Increased Cancer Risk in Children
A multinational cohort study (EPI-CT) conducted by Gomez et al. examined nearly one million individuals who underwent CT scans before age 22 across nine European countries. The study revealed a dose-response association between the cumulative radiation in bone marrow from CT scans and the risk of developing hematological malignancies, including those of lymphoid and myeloid lineage, with doses as low as 10 – 15 milligray (mGy). In addition, when comparing the number of CT procedures rather than the active bone marrow dose, patients who underwent more than one CT scan exhibited a 43% higher risk for hematological and lymphoid malignancies as compared to those who underwent only one CT scan. The excess relative risk for all hematological malignancies in children, adolescents, and young adults was 1.96 per 100 mGy, indicating almost a 2-fold increase in relative risk.
EPI-CT Study Findings
In addition, the researchers reported similar risk estimates for lymphoid and myeloid malignancies and acute lymphoma. The investigator’s analyses estimated an excess absolute risk of 17.7 per 100,000 person-years per 100 mGy, suggesting that for every 100,000 pediatric patients examined in a given day, 17 to 18 patients could potentially develop hematological malignancies within 12 years of an eight mGy mean exposure attributed to the ionizing radiation (Gomez et al., 2023). These results suggest that exposure to radiation from imaging procedures in pediatric patients can increase the risk of developing hematological malignancy, highlighting the importance of reducing unnecessary radiation exposure by being cautious and selective when recommending these studies to young patients.
Miglioretti et al. Study Findings
Similarly, Miglioretti et al. identified an elevated risk of radiation-induced cancer in children undergoing pediatric CT imaging. Miglioretti et al. conducted a retrospective observational study using data from over seven US healthcare systems from 1996 – 2010, including children younger than 15 years old who were examined via CT scans (152,419 – 371,095 children per year). The study found that cancer risks varied based on age, gender, and the region of the body being imaged. Younger patients and girls exhibited an increased risk for solid cancer (projected cases: 13.1 – 33.9 girls vs. 6.3 – 14.8 boys per 10,000 CT scans). Furthermore, abdomen/pelvis CT scans, which have a mean effective dose of 10.6 millisieverts (mSv) (same as 10.6 mGy) in children younger than 5 and 14.8 mSv in children 10-14 years old, had the highest risk for radiation-induced solid cancers, especially in the older children.
Pearce et al. Study Findings
Meanwhile, head CT scans, the most commonly performed pediatric CT, posed a higher risk of leukemia and brain cancer, particularly in children under five years old, which had a projected risk of 1.9 cases of leukemia per 10,000 head CT scans. The study projected that four million pediatric CT scans of the head, abdomen/pelvis, chest, or spine in the US per year could cause 4,870 future cancers. The majority of projected cancers in exposed girls are breast, thyroid, lung cancer, and leukemia, whereas in exposed boys, about half the projected cancers are in the brain, lung, colon cancer, and leukemia. Given that effective doses vary between 0.03 – 69.2 mSv, reducing the highest effective doses (25% upper quartile) might aid in potentially preventing over 43% of the projected cancers (Miglioretti et al., 2013). These projections highlight the potential long-term consequences of radiation exposure from CT imaging pediatric patients. Healthcare providers should carefully consider the benefits and necessity of these procedures, especially in the pediatric population, which displays the highest vulnerability to the effects of ionizing radiation due to their sensitivity and longer lifespan to develop cancer.

Cao et al. Meta-Analysis Findings
Additionally, Pearce et al. conducted a retrospective cohort study using data from the National Health Services (NHS) Centers in Great Britain between 1985 and 2002, where patients younger than 22 without a previous cancer diagnosis were included. Analysis of leukemia and brain tumors involved 178,604 and 176,587 people, respectively. Head CT scans constituted the majority of CTs (64%), followed by abdomen/pelvis (9%) and chest CT (7%). The study demonstrated a significant association between radiation doses from CT scans and subsequent incidents of leukemia and brain tumors. Patients who received a dose of 30 mGy had a 3.18 times higher risk of developing leukemia compared to those who received doses of less than five mGy.
Implications for Healthcare Providers
Compared to patients with a dose of less than five mGy, those receiving a dose of 50-74 mGy had a 2.82 times higher risk of developing brain tumors, and those receiving a dose of 50 mGy or more were 3.32 times as likely to develop brain tumors. This implies that exposure to 2-3 head CTs, resulting in a cumulative dose of approximately 60 mGy in the brain, increases the risk of developing brain tumors almost threefold in children below 15 years old. While exposure to 5-10 head CTs can lead to the accumulation of about 50 mGy in red bone marrow dose, tripling the risk of leukemia in children below 15 years of age. In addition, the study also identified statistically significant associations between CT scans and cancer subgroups, including gliomas, schwannomas, meningiomas, acute lymphoblastic leukemia, and myelodysplastic syndromes (Pearce et al., 2012).
Conclusion and Recommendations
CT scans are valuable medical diagnostic tools that can quickly detect tumors, injuries, and other health abnormalities. However, an extensive body of evidence demonstrates a dose-response relationship between cumulative radiation doses from CT scan exposure and the risk of developing radiation-induced malignancies, especially in children. Therefore, healthcare providers must exercise caution and prudence when recommending these procedures and participate in informed decision-making with the patient.
The multinational cohort study conducted by Bosch de Basea Gomez et al. demonstrated a positive association between cumulative radiation from CT scans and the risk of developing hematological malignancies in young individuals, highlighting the potential long-term consequences of repeated exposures to ionizing radiation from CT scans. Similarly, Miglioretti et al. identified an elevated risk of radiation-induced cancer in pediatric patients undergoing CT imaging, projecting that thousands of future cancer cases may occur annually in the United States as a result of failing to minimize effective doses. Pearce et al. study reinforced these findings by revealing a positive association between radiation doses from CT scans and subsequent incidents of leukemia and brain tumors in children. Finally, Cao et al. multi-continental meta-analysis emphasized that even in adults, cumulative radiation doses from CT scans are associated with a linear increase in cancer risks, with higher doses resulting in a rapid increase in cancer odds. These studies collectively provide ample and compelling evidence that even low to moderate doses of ionizing radiation from CT scans can significantly increase the long-term risk of hematological malignancies, solid cancers, leukemia, and brain tumors.
Healthcare providers must carefully weigh the benefits and risks of CT imaging, especially in vulnerable populations such as pediatric patients and individuals undergoing repeated scans. Alternative imaging techniques such as ultrasound and magnetic resonance imaging should be considered in order to make a diagnosis whenever possible. Patients should also be thoroughly informed about the associated risks before undergoing CT procedures, and discussion with the physician regarding any concerns and questions should be encouraged. Additionally, radiation dose optimization strategies are necessary to reduce potential health risks and improve patient safety during CT scans to enhance quality care. Although CT scans are associated with an increased risk of developing cancer, they remain an extremely valuable resource in diagnostic medicine, particularly in emergency cases where prompt diagnosis is needed to take appropriate action. Therefore, their usefulness should not be diminished and underappreciated.
References
Bosch de Basea Gomez, M., Thierry-Chef, I., Harbron, R., Hauptmann, M., Byrnes, G., Bernier, M.-O., Le Cornet, L., Dabin, J., Ferro, G., Istad, T. S., Jahnen, A., Lee, C., Maccia, C., Malchair, F., Olerud, H., Simon, S. L., Figuerola, J., Peiro, A., Engels, H., … Cardis, E. (2023). Risk of hematological malignancies from CT radiation exposure in children, adolescents and young adults. Nature Medicine, 29(12), 3111–3119. https://doi.org/10.1038/s41591-023-02620-0
Cao, C.-F., Ma, K.-L., Shan, H., Liu, T.-F., Zhao, S.-Q., Wan, Y., Jun-Zhang, null, & Wang, H.-Q. (2022). CT Scans and Cancer Risks: A Systematic Review and Dose-response Meta-analysis. BMC Cancer, 22(1), 1238. https://doi.org/10.1186/s12885-022-10310-2
Computed Tomography (CT). (2022). National Institute of Biomedical Imaging and Bioengineering. Retrieved February 12, 2024, from https://www.nibib.nih.gov/science-education/science-topics/computed-tomography-ct
Miglioretti, D. L., Johnson, E., Williams, A., Greenlee, R. T., Weinmann, S., Solberg, L. I., Feigelson, H. S., Roblin, D., Flynn, M. J., Vanneman, N., & Smith-Bindman, R. (2013). The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatrics, 167(8), 700–707. https://doi.org/10.1001/jamapediatrics.2013.311
Pearce, M. S., Salotti, J. A., Little, M. P., McHugh, K., Lee, C., Kim, K. P., Howe, N. L., Ronckers, C. M., Rajaraman, P., Sir Craft, A. W., Parker, L., & Berrington de González, A. (2012). Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: A retrospective cohort study. Lancet (London, England), 380(9840), 499–505. https://doi.org/10.1016/S0140-6736(12)60815-0
Figure 1: https://www.sanjuanmri.net/wp-content/uploads/2023/08/mri.jpg
Figure 3: https://upload.wikimedia.org/wikipedia/commons/9/96/CT_of_a_normal_brain_%28thumbnail%29.png


[…] A. Garriga García assesses the impact of CT scans on cancer risk (p. […]
LikeLike