
This article was published on Arbona Health Hub Volume 1 Issue 1 (ISSN: 3065-5544).
Health Warning: Fasting is a serious medical practice which should be approached with strong consideration to individual health conditions/nutritional requirements. Always consult a healthcare professional if you intend to begin fasting, especially for prolonged periods of time.
Introduction
Fasting is the practice of abstaining from or limiting food and/or drink consumption over a certain period of time. It has been a part of various cultural/religious traditions for centuries and can be utilized towards spiritual, social, and health purposes. For example, many people incorporate fasting into their regular routines or as a part of specific religious observances. Fasting periods may range from a few hours to several days, depending on an individual’s needs. A fast may involve complete abstinence from food and water (often referred to as “dry fasting”) or it may allow for consumption of certain types of food/drink (e.g. water fasting).[1]
Therapeutic Fasting
The roots of fasting trace back to ancient cultures where it held spiritual significance, serving as a means of purification, penance, and connection with the divine. In ancient Greece, fasting was believed to promote healing and detoxification. Hippocrates, often lauded as the father of modern medicine, frequently prescribed fasting as a remedy for various ailments.[2]
In the early 20th century, Dr. Otto Buchinger and Dr. Arnold Ehret advocated for the use of fasting in therapeutic settings. Their efforts drew the attention of the scientific community towards fasting as a potential treatment for chronic conditions such as obesity, diabetes, and hypertension.[2,3]
Consequently, modern researchers have focused efforts towards unraveling the physiological impacts of fasting. Several studies have shown that fasting can result in health benefits, such as weight loss and improved insulin sensitivity. [1,4] Other studies point to the connection between fasting and immune function, noting that time-restricted feeding clinical protocols may result in reduced inflammation and enhanced cellular repair processes (autophagy).[4]
This article will outline this immune connection, focusing specifically on inflammation, and how it may be managed through fasting clinical protocols.
Fasting and the Immune System
Immunometabolism is a field of study which explores the intricate relationship between metabolism and immune cell function. It focuses on how metabolic pathways regulate the function of immune cells, and how immune responses, in turn, influence metabolic processes in the body.[5] Today, researchers remain fascinated with the potential to use fasting to modulate the immune system. To do so, the pathways which link the immune system to metabolism are actively under investigation.
A substantial focus has been placed on nicotinamide adenine dinucleotide (NAD+), a molecule which is widely used in metabolic reactions and throughout the body.[5]
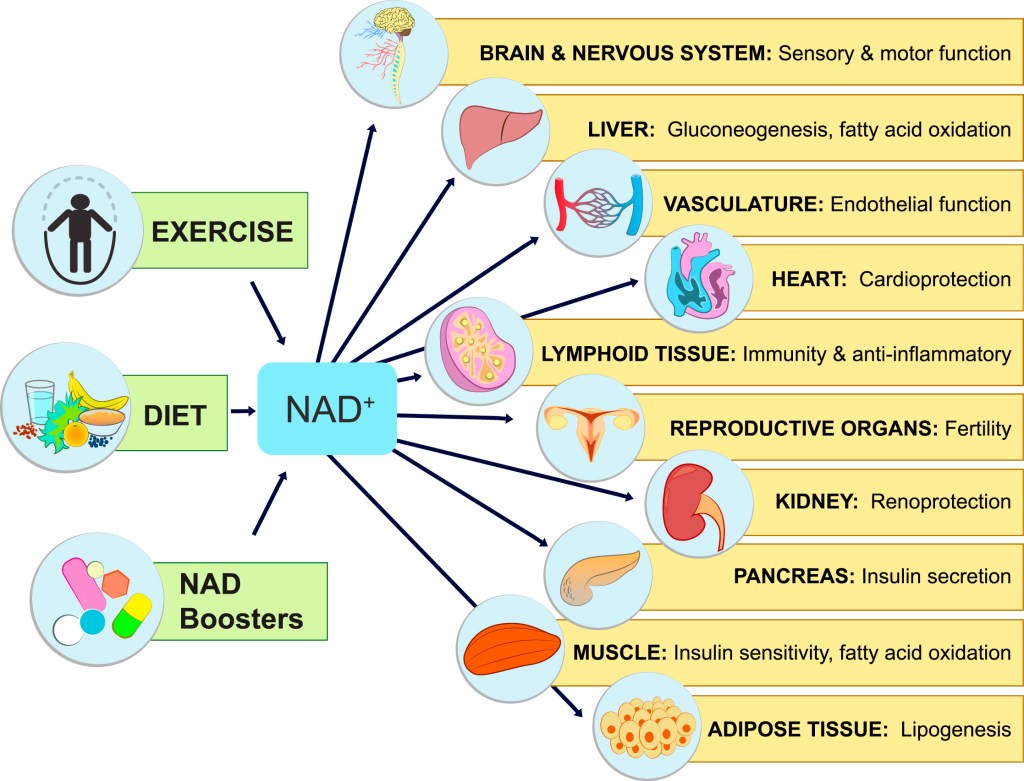
Fasting has been shown to robustly increase levels of NAD+ in the body.[5] This “NAD+-boosting” is believed to elicit anti-inflammatory effects through the following mechanisms:
- Activation of Sirtuin enzymes → Sirtuins are a family of enzymes involved in the regulation of inflammation. They rely on NAD+ to function, so NAD+ boosting is believed to improve their inflammation regulation function.[5]
- Inhibition of PARP enzymes → Poly(ADP-ribose) polymerases (PARPs) are enzymes that consume NAD+ during DNA repair processes. Excessive PARP activation can deplete cellular NAD+ levels, leading to increased inflammation. Inhibiting PARP activity helps preserve NAD+ levels and reduces inflammation.[4]
- Reduction of Oxidative Stress → NAD+ is a key regulator of reduction/oxidation reactions in cells. Oxidative stress can promote inflammation by activating pro-inflammatory signaling pathways. Boosting NAD+ can help maintain adequate NAD+ levels, allowing cells to better counteract oxidative stress and mitigate inflammation.[4]
Numerous other biological mechanisms linking fasting and reduced inflammation have been reported. For example, in a recent paper published in Cell Reports, researchers found that higher levels of the important metabolite, arachidonic acid, following fasting can result in active inhibition of pro-inflammatory mediators such as the NLRP3 inflammasome.[6]
A 2019 study published in Cell notes that reducing dietary intake via fasting can have a regulatory effect on levels of circulating monocyte pool available for inflammatory responses. Moreover, it was found that fasting has the potential to improve inflammation without compromising immunity against pathogenic microbes.[7] Collectively, these findings highlight the value fasting protocols may provide in anti-inflammatory treatment regimes.
Implications for Patients
Understanding the links between the immune system and metabolism in the context of fasting is an important task with important implications for patients. Identification of new immunometabolic pathways may allow for the development of novel therapeutic agents/strategies for inflammation treatment. For example, if a robust pathway linking NAD+ boosting to reduced inflammation is outlined by researchers, this information could be used to validate the use of NAD+-boosting agents such as nicotinamide riboside, succinic acid, resveratrol, etc. for patients burdened with inflammatory disease.
With further research, fasting itself may become a more common strategy prescribed by medical professionals to manage the inflammation of their patients.
Conclusion
Fasting has deep historical roots in various cultures and traditions, and its application in modern healthcare continues to evolve with ongoing research and clinical practice.
The relationship between fasting, NAD+ boosting, and improved immune health is actively being outlined by researchers. There is considerable evidence to suggest that NAD+ boosting contributes to an anti-inflammatory environment by regulating various molecular pathways involved in inflammation, enhancing cellular metabolism, and preserving tissue homeostasis.
However, while fasting may offer benefits for immune health by promoting cellular renewal, reducing inflammation, and modulating immune responses, prolonged or extreme fasting should be approached with caution, as it may have detrimental effects on immune function.
As with any lifestyle or dietary change, it is imperative to consider one’s personal health conditions and consult with a healthcare professional before beginning a fasting regimen.
References
- Patterson R.E., Laughlin G.A., LaCroix A.Z., Hartman S.J., Natarajan L., Senger C.M., Martínez M.E., Villaseñor A., Sears D.D., Marinac C.R., Gallo L.C. (2015). Intermittent Fasting and Human Metabolic Health. Journal of the Academy of Nutrition and Dietetics, 115(8), 1203–1212. https://doi.org/10.1016/j.jand.2015.02.018
- Kerndt, P. R., Naughton, J. L., Driscoll, C. E., & Loxterkamp, D. A. (1982). Fasting: The History, Pathophysiology and Complications. Western Journal of Medicine, 137(5), 379.
- Boschmann, M., Michalsen, A. (2013) Fasting Therapy – Old and New Perspectives. Research in Complementary and Classical Natural Medicine, 20(6), 410–411. https://doi.org/10.1159/000357828
- Rajman, L., Chwalek, K., & Sinclair, D. A. (2018). Therapeutic Potential of NAD-Boosting Molecules: The In Vivo Evidence. Cell Metabolism, 27(3), 529–547. https://doi.org/10.1016/j.cmet.2018.02.011
- Perry, J. M., Wu, J., Bley, M., Steans, R. S., Meadows, A. M., Huffstutler, R. D., Tian, R., Griffin, J. L., & Sack, M. N. (2024). Nicotinamide Riboside Augments Human Macrophage Migration via SIRT3-Mediated Prostaglandin E2 Signaling. Cells, 13(5), 455. https://doi.org/10.3390/CELLS13050455
- Pereira, M., Liang, J., Edwards-Hicks, J., Meadows, A. M., Hinz, C., Liggi, S., Hepprich, M., Mudry, J., Han, K., Griffin, J. L., Fraser, I., Sack, M. N., Hess, C., & Bryant, C. E. (2024). Arachidonic acid inhibition of the NLRP3 inflammasome is a mechanism to explain the anti-inflammatory effects of fasting. Cell Reports, 43(2), 113700. https://doi.org/10.1016/J.CELREP.2024.113700
- Jordan, S., et al. (2019). Dietary intake regulates the circulating inflammatory monocyte pool. Cell, 178(5), 1102. https://doi.org/10.1016/J.CELL.2019.07.050


[…] plant-based (as discussed by Avery), vegetarian, low-carb, intermittent fasting (as discussed by Russell), Mediterranean diet, etc. • Aim to minimize consumption of processed foods. Processed foods have […]
LikeLike
[…] S. Steans looks into the connection between fasting and immune health (p. […]
LikeLike