This article was published on Arbona Health Hub Volume 2 Issue 1 (ISSN: 3065-5544).
Oral health plays a vital role in overall well-being. Its importance often goes beyond just having a bright white smile. Why is oral health so important? According to the World Health Organization (WHO), nearly 3.5 billion people are affected by oral diseases. The most prevalent condition is dental caries, affecting an estimated 2.5 billion people with permanent teeth. Severe periodontal disease, also known as gum disease, impacts approximately 1 billion people, leading to tooth loss or edentulism, especially among older adults (WHO, 2022).
Oral cancers, particularly oropharyngeal cancer, are on the rise in many countries, being the 16th most common neoplasm worldwide. Risk factors such as tobacco use, alcohol consumption, and human papilloma virus (HPV) infection are contributing to this increase. Oropharyngeal cancer accounts for over 377,000 new cases and more than 177,000 deaths annually worldwide (Miranda-Filho & Bray, 2020). Untreated oral diseases can not only cause local effects such as pain, infections, or difficulty eating, but can also contribute to broader systemic health issues (Scannapieco & Cantos, 2016).
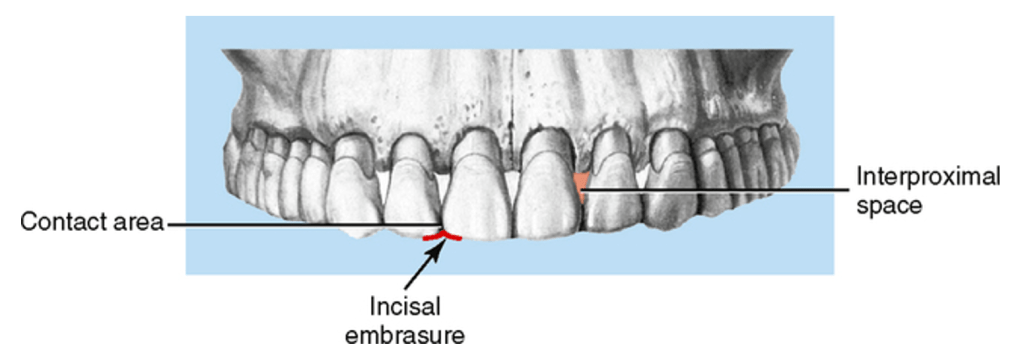
The challenge we face today is the misconception that tooth brushing alone is sufficient. In reality, brushing often focuses only on front-facing and visible areas, overlooking lateral (interproximal and incisal) areas as shown in Figure 1. These areas between the teeth and along the gumline are where plaque and bacteria can accumulate unnoticed, and they are the most common sites for the formation of caries (Deinzer et al., 2018). This oversight can contribute to the progression of gum disease, tooth decay and entry of harmful bacteria into the bloodstream. This increases the risk for systemic conditions such as cardiovascular disease, diabetes, and adverse pregnancy outcomes (Weidlich et al., 2008). Raising awareness about the connection between oral health and overall well-being is key to helping individuals understand that taking care of their teeth is a long-term investment in their health.
Connection Between Oral Health and Overall Health
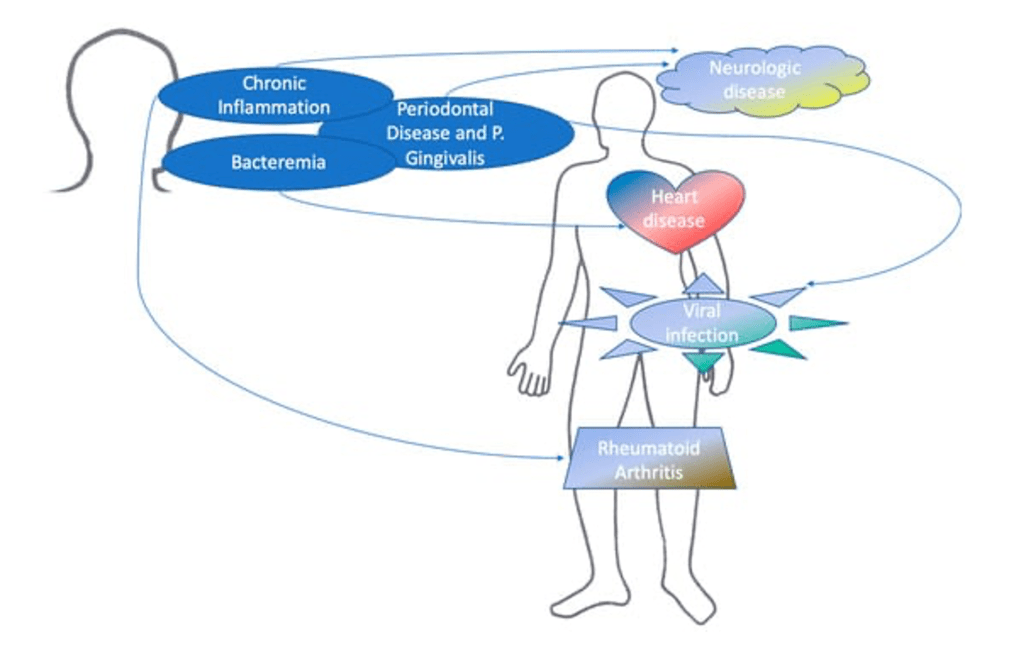
While the importance of oral health is often recognized in terms of appearance, its impact on overall health cannot be overlooked. The foundation or overall health. Scientific research has shown that poor oral health can contribute to systemic conditions such as cardiovascular diseases and diabetes, lung diseases, and obstetric complications (Fiorillo, 2019). Emerging studies emphasize the relationship between periodontal disease and systemic health is linked to diabetes, metabolic syndrome, obesity, eating disorders, liver disease, cardiovascular disease, Alzheimer disease, rheumatoid arthritis, and even cancer (Kapila, 2021). For instance:
- Cardiovascular disease: Inflammation from periodontal disease can lead to atherosclerosis, increasing the risk of heart attacks and strokes by promoting plaque buildup in blood vessels (Lockhart et al., 2012).
- Diabetes: High blood sugar can weaken the immune system and worsen gum disease, while severe gum disease can make it harder to control blood glucose levels (NIH, 2024).
- Alzheimer’s disease: Porphyromonas gingivalis, a key pathogen in periodontitis, has been found in the brains of Alzheimer’s patients and is associated with increased neuroinflammation (Dominy et al., 2019).
- Rheumatoid arthritis: Periodontal disease may worsen rheumatoid arthritis by increasing systemic inflammation. Porphyromonas gingivalis can trigger immune responses linked to the condition (Bingham & Moni, 2013).
- Cancer: Chronic inflammation and exposure to oral bacteria have been linked to increased risk of oral, pancreatic, and other cancers (Michaud et al., 2013).
These oral conditions can affect systemic health, as shown in Figure 2. To address these complex relationships, a comprehensive approach to patient care is necessary. This approach involves evaluating not just oral health but also considering broader systemic health factors, such as lifestyle habits, medical history, and risk factors for chronic diseases. Integrating both oral and systemic health assessments ensures early detection of potential health issues, promotes more effective prevention strategies, and leads to improved health outcomes. For example, treating periodontal disease in diabetic patients can help manage blood sugar levels, and addressing oral infections may reduce the risk of cardiovascular events. A holistic approach allows healthcare providers to tailor more effective, personalized care for patients.
Prevention of Serious Conditions
To prevent serious systemic conditions, it is crucial to revisit the basics and learn the proper way to perform toothbrushing. A study highlighted that tooth brushing, when done incorrectly, is not enough to ensure good oral health. It is crucial to maintain a high quality brushing by giving attention to the occlusal and lateral surfaces, which are often forgotten (Deinzer et al., 2018). Failing to properly clean these areas, can lead to high vulnerability to decay, specifically in the lateral and proximal surfaces of the teeth.
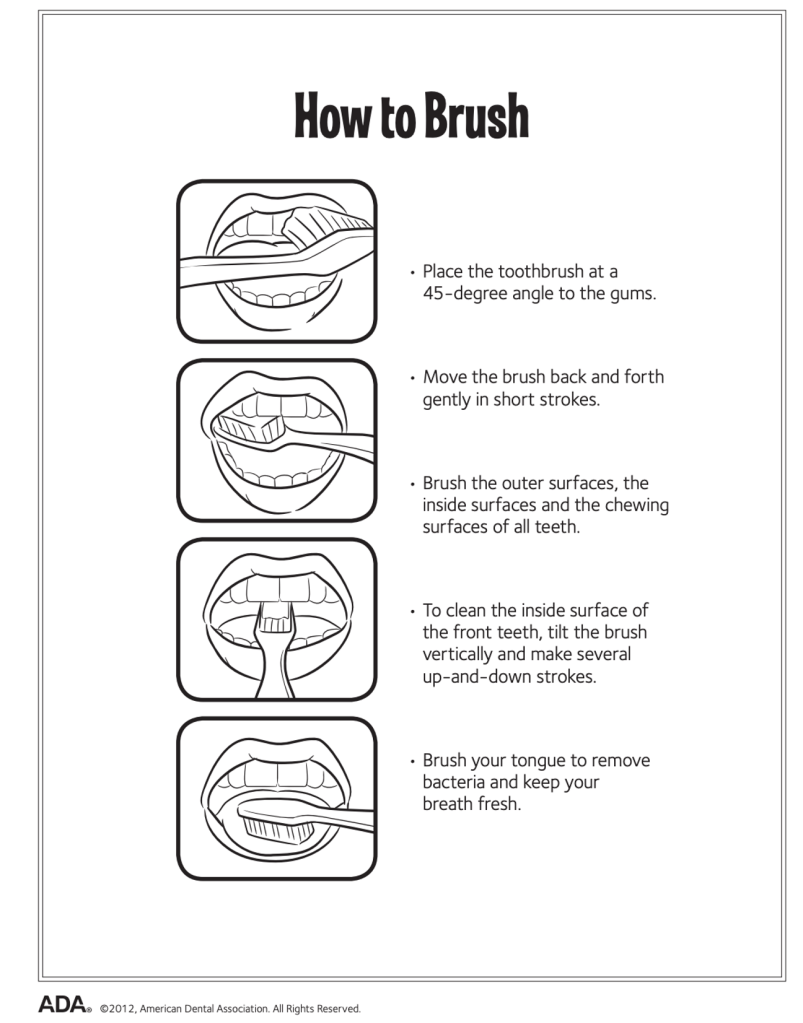
To maintain optimal oral health and prevent systemic diseases, it is essential to learn that brushing the teeth should be twice a day for two minutes each time as shown in Figure 3. The toothbrush should be positioned at a 45 degree angle to the gums, gently moving the brush back and forth (American Dental Association, 2012). Additionally, cleaning between teeth with floss daily and adding a water flosser can provide extra benefits. It is also important to replace the toothbrush every three to four months (Mayo Clinic, 2024). Regular dental check-ups and professional cleaning are crucial for maintaining overall oral health. By following these practices, individuals can help prevent dental issues and further systemic diseases.
Conclusion
Addressing the direct link between oral health and systemic conditions is essential for raising awareness. Oral health is not just about a bright smile; it plays a crucial role in overall well-being. Untreated oral diseases can lead to local issues like pain and infections, but they can also contribute to serious systemic health problems, including cardiovascular disease, diabetes, and even cancer. Recognizing the importance of oral health and its impact on general health is key to improving health outcomes, raising awareness, and fostering a population that is more informed about their oral care. Prioritizing oral health is essential for preventing serious health issues and improving quality of life.
References
Image credits:
- Figure 1. Adapted from Themes, U. (2015, January). 3: Fundamental and preventive curvatures: proximal alignment of the teeth and protection of the periodontium. Pocket Dentistry. https://pocketdentistry.com/3-fundamental-and-preventive-curvatures-proximal-alignment-of-the-teeth-and-protection-of-the-periodontium/
- Figure 2. Adapted from Fiorillo, L. (2019). Oral Health: The First Step to Well-Being. Medicina, 55(10), 676. https://doi.org/10.3390/medicina55100676
- Figure 3. Adapted from Brushing your teeth. (n.d.). MouthHealthy – Oral Health Information From the ADA. https://www.mouthhealthy.org/all-topics-a-z/brushing-your-teeth
Sources:
- World Health Organization: WHO. (2025, March 17). Oral health. https://www.who.int/news-room/fact-sheets/detail/oral-health
- Miranda-Filho, A., & Bray, F. (2020). Global patterns and trends in cancers of the lip, tongue and mouth. Oral Oncology, 102, 104551. https://doi.org/10.1016/j.oraloncology.2019.104551
- Scannapieco, F. A., & Cantos, A. (2016). Oral inflammation and infection, and chronic medical diseases: implications for the elderly. Periodontology 2000, 72(1), 153–175. https://doi.org/10.1111/prd.12129
- Deinzer, R., Ebel, S., Blättermann, H., Weik, U., & Margraf-Stiksrud, J. (2018). Toothbrushing: to the best of one’s abilities is possibly not good enough. BMC Oral Health, 18(1). https://doi.org/10.1186/s12903-018-0633-0
- Weidlich, P., Cimões, R., Pannuti, C. M., & Oppermann, R. V. (2008). Association between periodontal diseases and systemic diseases. Brazilian Oral Research, 22(suppl 1), 32–43. https://doi.org/10.1590/s1806-83242008000500006
- Fiorillo, L. (2019). Oral Health: The First Step to Well-Being. Medicina, 55(10), 676. https://doi.org/10.3390/medicina55100676
- Kapila, Y. L. (2021). Oral health’s inextricable connection to systemic health: Special populations bring to bear multimodal relationships and factors connecting periodontal disease to systemic diseases and conditions. Periodontology 2000, 87(1), 11–16. https://doi.org/10.1111/prd.12398
- Lockhart, P. B., et al. (2012). Periodontal disease and atherosclerotic vascular disease: Does the evidence support an independent association? Circulation, 125(20), 2520–2544. https://doi.org/10.1161/cir.0b013e31825719f3
- Diabetes & oral health. (National Institute of Dental and Craniofacial Research, 2024). https://www.nidcr.nih.gov/health-info/diabetes
- Dominy, S. S., et al. (2019). Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Science Advances, 5(1). https://doi.org/10.1126/sciadv.aau3333
- Bingham, C. O., & Moni, M. (2013). Periodontal disease and rheumatoid arthritis. Current Opinion in Rheumatology, 25(3), 345–353. https://doi.org/10.1097/bor.0b013e32835fb8ec
- Michaud, D. S., et al. (2012). Plasma antibodies to oral bacteria and risk of pancreatic cancer in a large European prospective cohort study. Gut, 62(12), 1764–1770. https://doi.org/10.1136/gutjnl-2012-303006
- Themes, U. (2015, January). 3: Fundamental and preventive curvatures: proximal alignment of the teeth and protection of the periodontium. Pocket Dentistry. https://pocketdentistry.com/3-fundamental-and-preventive-curvatures-proximal-alignment-of-the-teeth-and-protection-of-the-periodontium/
- Brushing your teeth. (n.d.). MouthHealthy – Oral Health Information From the ADA. https://www.mouthhealthy.org/all-topics-a-z/brushing-your-teeth
- Oral health: A window to your overall health. (March, 2024). Mayo Clinic. https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/dental/art-20047475

