This article was published on Arbona Health Hub Volume 2 Issue 1 (ISSN: 3065-5544).
Heart disease is the leading cause of death for both men and women. According to the American Heart Association’s latest statistics, 40.3% of cardiovascular deaths are caused by coronary heart disease. Atherosclerotic cardiovascular disease (ASCVD) is a major causes of coronary heart disease and involves the buildup of plaque within arteries, which can obstruct the passage of blood – and therefore oxygen – to organs.
Menopause and Cardiovascular Risk
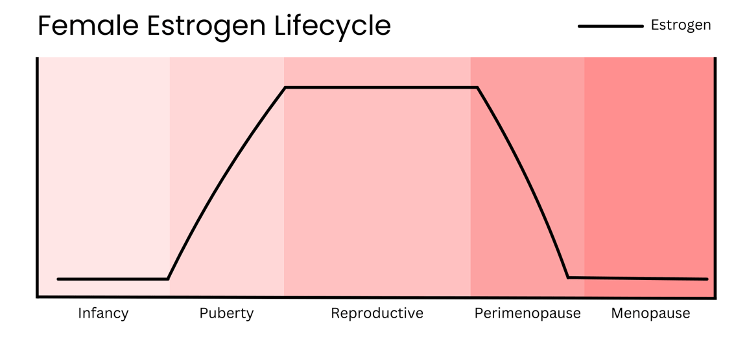
Women have a lower prevalence of ASCVD than men before menopause. However, after menopause, the prevalence of ASCVD in women increases and even surpasses that of men. Natural menopause typically occurs between the ages of 45 and 55 for most women, which coincides with the timing of a significant increase in ASCVD risk (El Khoudary et al., 2020). Of course, factors such as race and presence of chronic diseases, like diabetes, also influence the onset of cardiovascular disease in women. When considering why this significant increase occurs after menopause, the first factor that may come to mind is the change in hormone composition. While estrogen plays a key role in this postmenopausal shift in cardiovascular health, there are other components that may contribute to this change.
The transition into menopause includes a decline in estrogen, alterations in body fat and lipid composition, sleep pattern disruption, and appearance of vasomotor symptoms, such as hot flashes and night sweats. These factors all impact cardiovascular health in some way, but research on some of them remains limited. Atherosclerosis is the process of plaque formation in arteries. This plaque is composed of the buildup of fat, LDL cholesterol, and other substances. Several studies on mice and human models have found that estrogen has protective effects against plaque formation. Estrogen induces nitric oxide production via the estrogen receptor a (ERa) in mice (Darblade et al., 2002). Nitric oxide induces vasodilation in blood vessels, maintains healthy endothelial function, and has anti-inflammatory properties that help prevent atherosclerosis. Estrogen has also been found to reduce circulating levels of low-density lipoprotein (LDL), also known as “bad cholesterol”, by upregulating LDL receptors in the liver (Persson et al., 2012). The metabolic changes that occur during menopause alter lipid composition. Postmenopausal women present with increased concentrations of LDL cholesterol and inflammatory biomarkers that promote the formation of plaque (Wang et al., 2018). Higher levels of LDL cholesterol in blood mean a higher rate of fat deposition in arteries and, therefore, development of atherosclerosis.
Current Treatment and Prevention Strategies
Regarding effective treatment and prevention options much remains to be studied and explored. Current strategies focus on lifestyle modifications and pharmacotherapy. Smoking cessation, diet, and exercise are the primary recommendations for reducing ASCVD risk. For women with predisposing conditions such as hypertension, diabetes – or those who have already begun to develop ASCVD – pharmacological therapy with blood pressure and lipid-lowering medications is indicated. These interventions are the standard management strategies for ASCVD in general and have been proven effective; however, none are specifically tailored for women going through menopause.
Hormone Replacement Therapy (HRT) and Controversy
Although post-menopausal increase in ASCVD risk is linked to estrogen decline, therapy targeting this decline remains controversial and has not been approved for cardiovascular disease prevention. This approach, known as hormone replacement therapy (HRT), involves the administration of estrogen to relieve menopausal symptoms such as hot flashes and night sweats. Currently, the American Heart Association advises against the use of HRT for cardiovascular disease prevention. Research has shown that HRT as a secondary prevention method for coronary vascular disease (CVD) does not significantly reduce cardiovascular disease and actually increases the risk of adverse events such as breast cancer, stroke, and thromboembolism (Kim et al., 2020).
Some research suggests that when HRT is initiated before menopause in women under 60 years of age, it may reduce cardiovascular disease and mortality (Hodis and Mack, 2022). This idea, known as the “timing hypothesis”, is based on estrogen’s protective effects on blood vessels, including vasodilation, inflammatory control, and lipid level reduction. The thought behind this hypothesis is that if these protective effects are administered before menopause exerts its damaging effects on blood vessel health, then HRT could serve as a primary prevention method against cardiovascular disease in women. However, there is insufficient research to support this, and the positive results observed are not significant enough to outweigh the risks associated with HRT. There aren’t any other therapeutic strategies that specifically target the hormonal changes linking menopause and heart disease, highlighting the need for further research and innovation.
Gaps in Research and Diagnosis
Although estrogen decline and the metabolic alterations that occur during menopause are evident contributors to the increase ASCVD risk in women, other factors must also be considered when evaluating prevalence. Cardiovascular disease in premenopausal and postmenopausal women is often underdiagnosed due to the difference in symptomatic presentation and the lack of research on female health topics. Women are generally less aware of the symptoms they should look out for and how common cardiovascular disease is among women.
Men typically present with the classic chest pain traditionally associated with heart disease, while women experience more atypical symptoms such as abdominal and jaw pain, nausea, and fatigue. These symptoms are frequently overlooked, not only by patients, but sometimes even by medical professionals. Education on how cardiovascular disease affects women could improve patient awareness, helping them recognize the signs and symptoms that indicate when to seek medical attention.
In heart disease, timely intervention is key to preventing progression and mortality. It is also important to acknowledge the lack of research for strategies targeted towards the prevention of post-menopausal heart disease and women’s cardiovascular health in general. Addressing the unique risk factors and knowledge gaps associated with cardiovascular disease in women is essential for improving diagnosis, prevention, and treatment strategies, particularly during and after the menopausal transition.
References
Darblade, B., Pendaries, C., Krust, A., Dupont, S., Fouque, M.-J., Rami, J., Chambon, P., Bayard, F., & Arnal, J.-F. (2002). Estradiol alters nitric oxide production in the mouse aorta through the α-, but not β-, estrogen receptor. Circulation Research, 90(4), 413–419. https://doi.org/10.1161/hh0402.105096
El Khoudary, S. R. (2023). The menopause transition: A critical stage for cardiovascular disease risk acceleration in women. Menopause. https://doi.org/10.1097/gme.0000000000002172
Hodis, H. N., & Mack, W. J. (2022). Menopausal hormone replacement therapy and reduction of all-cause mortality and cardiovascular disease. The Cancer Journal, 28(3), 208–223. https://doi.org/10.1097/ppo.0000000000000591
Kim, J.-E., Chang, J.-H., Jeong, M.-J., Choi, J., Park, J., Baek, C., Shin, A., Park, S. M., Kang, D., & Choi, J.-Y. (2020). A systematic review and meta-analysis of effects of menopausal hormone therapy on cardiovascular diseases. Scientific Reports, 10(1). https://doi.org/10.1038/s41598-020-77534-9
More than half of U.S. adults don’t know heart disease is leading cause of death, despite 100-year reign. American Heart Association. (2024, January 24). https://newsroom.heart.org/news/more-than-half-of-u-s-adults-dont-know-heart-disease-is-leading-cause-of-death-despite-100-year-reign
Persson, L., Henriksson, P., Westerlund, E., Hovatta, O., Angelin, B., & Rudling, M. (2012). Endogenous estrogens lower plasma PCSK9 and LDL cholesterol but not lp(a) or bile acid synthesis in women. Arteriosclerosis, Thrombosis, and Vascular Biology, 32(3), 810–814. https://doi.org/10.1161/atvbaha.111.242461
Roeters van Lennep, J. E., Tokgözoğlu, L. S., Badimon, L., Dumanski, S. M., Gulati, M., Hess, C. N., Holven, K. B., Kavousi, M., Kayıkçıoğlu, M., Lutgens, E., Michos, E. D., Prescott, E., Stock, J. K., Tybjaerg-Hansen, A., Wermer, M. J., & Benn, M. (2023). Women, lipids, and atherosclerotic cardiovascular disease: A call to action from the European Atherosclerosis Society. European Heart Journal, 44(39), 4157–4173. https://doi.org/10.1093/eurheartj/ehad472
Wang, Q., Ferreira, D. L., Nelson, S. M., Sattar, N., Ala-Korpela, M., & Lawlor, D. A. (2018). Metabolic characterization of menopause: Cross-sectional and longitudinal evidence. BMC Medicine, 16(1). https://doi.org/10.1186/s12916-018-1008-8

