Introduction
The San Juan Metropolitan Area (SJMA) of Puerto Rico has a remarkably high prevalence of overweight and obesity (77.4%). This is substantially higher than the mainland U.S. adult population rate (68.8%). According to local data, women are more likely to have clinical obesity, while men are more likely to be overweight. This expanding public health crisis is driven by sedentary lifestyles, genetic predispositions, and local socioeconomic and sociocultural dynamics (SEC) (Pérez et al., 2013).
Metabolic Syndrome (MetS) is defined by the presence of at least three cardiometabolic risk factors, including elevated triglycerides, hypertension, hyperglycemia, increased waist circumference, and reduced HDL-C cholesterol, and is closely linked to obesity (NHLBI, 2022). MetS dramatically raises the risk of diseases like type 2 diabetes mellitus (T2DM) and cardiovascular disease (CVD) (Wilson et al., 2005).
Due to the high prevalence of obesity and MetS, Puerto Rican surgical patients are more likely to experience perioperative complications. Developing effective, evidence-based perioperative strategies requires an understanding of the biological mechanisms through which obesity and MetS influence wound healing and infection susceptibility.
Pathophysiology: Obesity, MetS, and Wound Healing
In addition to delaying wound healing and raising the risk of infection, obesity and MetS disrupt the normal tissue repair pathway by encouraging chronic low-grade inflammation, impaired coagulation, and microvascular dysfunction. These patients demonstrate elevated levels of high-sensitivity C-reactive protein (hsCRP), a biomarker of systemic inflammation. Chronically elevated CRP reflects persistent inflammation that can dysregulate immune responses and delay the transition from inflammation to tissue repair, resulting in slower wound healing (Pinchuk et al., 2024; Khaled & El-Din, 2024).
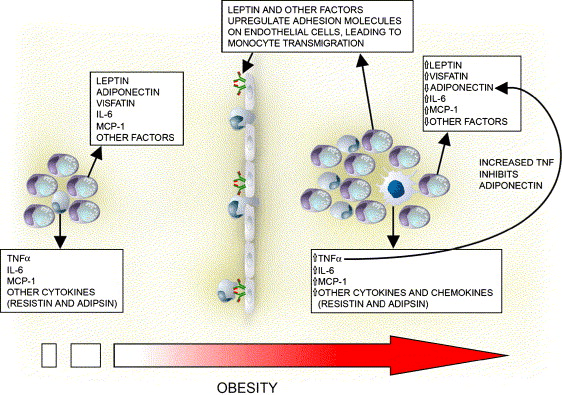
Beyond elevated CRP, obesity is also marked by increased secretion of inflammatory adipokines such as TNF-α, IL-6, and MCP-1 from adipocytes and infiltrating macrophages. These mediators amplify chronic low-grade inflammation and contribute to endothelial activation, immune dysregulation, and impaired wound healing (Fantuzzi, 2005) (see Figure 1).
Coagulation dysregulation further complicates tissue repair. Patients with obesity and MetS frequently exhibit elevated fibrinogen and plasminogen activator inhibitor-1 (PAI-1) levels. While these factors are essential for clot formation and provisional wound stabilization, chronic elevation affects the physiological balance needed for effective healing. Excess fibrinogen promotes a pro-thrombotic state, and increased PAI-1 inhibits fibrinolysis. Together, these changes create a hypofibrinolytic environment that can reduce tissue perfusion, prolong clot persistence, and impair tissue remodeling (Kearney et al., 2021; Sleiman et al., 2021).
Obesity and MetS impair vascular function in part through perivascular adipose tissue (PVAT) dysfunction. PVAT is the fat surrounding blood vessels that assists in regulating vascular tone and supporting healthy blood flow by releasing relaxing factors. In obesity, PVAT becomes inflamed and stressed, losing its protective role. This leads to increased vascular resistance and reduced tissue perfusion, which limits the delivery of oxygen and nutrients necessary for effective wound repair (Aoqui et al., 2014).
Surgical Outcomes in Patients with Obesity and MetS
Obesity is recognized as a significant surgical risk factor, particularly in gastroenterological procedures, due to its impact on both operative and postoperative outcomes. Higher body mass index (BMI) is consistently associated with prolonged operative times across surgeries such as esophagectomy, gastrectomy, hepatectomy, pancreaticoduodenectomy, and colorectal resection. Longer operative duration increases the risk of short-term complications, including surgical site infections, anastomotic leakage, pancreatic fistula, and pulmonary complications (Ri et al., 2018).
These surgical risks are further amplified when obesity coexists with MetS, as the combination of insulin resistance, hypertension, dyslipidemia, and central adiposity contributes to systemic inflammation, endothelial dysfunction, and coagulation abnormalities. Patients with MetS undergoing major surgeries, such as coronary artery bypass grafting, demonstrate significantly higher operative mortality and adverse postoperative outcomes compared to those without MetS, indicating increased perioperative risk related to metabolic instability (Echahidi et al., 2007). Such disruptions in inflammation, coagulation, and perfusion likely connect to the increased operative complications observed in patients with obesity and MetS.
Strategies for Perioperative Optimization
Optimizing outcomes in obese surgical patients requires proactive strategies across the perioperative course. Preoperatively, risk stratification tools such as the Edmonton Obesity Staging System help identify patients most vulnerable to complications. Intraoperatively, minimally invasive approaches and careful anesthetic management can reduce operative stress and blood loss. Postoperatively, Enhanced Recovery After Surgery (ERAS) protocols, emphasizing early mobilization, targeted physiotherapy, and adequate nutrition, have been shown to shorten hospital stay and reduce complications (Plassmeier et al., 2021). Beyond the hospital, long-term improvements in nutrition, exercise, and sleep hygiene are critical to lowering metabolic risk and enhancing recovery.
Discussion
The high prevalence of obesity and Metabolic Syndrome (MetS) in Puerto Rico presents significant implications for surgical care, particularly because the pathophysiological alterations present in these conditions intersect with key phases of perioperative physiology. As outlined earlier, chronic inflammation, coagulation imbalance, endothelial dysfunction, and impaired tissue perfusion collectively worsen postoperative outcomes. The complexity of these mechanisms helps explain why obese and metabolically unstable patients demonstrate higher rates of surgical site infections, delayed wound healing, and cardiopulmonary complications. In Puerto Rico, where obesity rates surpass those of the mainland U.S., the clinical burden on surgical services is significantly high. A population with a 77.4% combined overweight/obesity prevalence increases the number of high-risk surgical candidates, particularly those undergoing abdominal, thoracic, and vascular procedures. Moreover, socioeconomic and sociocultural (SEC) factors, including limited access to nutrient-dense foods, high prevalence of sedentary lifestyles, and cultural dietary patterns, create systemic barriers to preoperative optimization. These factors may limit patients’ ability to engage in lifestyle modification prior to elective procedures, making metabolic instability an even more well-established predictor of poor surgical outcomes on the island.
The literature supports that prolonged operative times in obese patients reflect both technical challenges and broader physiological disadvantages. For example, increased intra-abdominal adiposity complicates exposure and visualization, resulting in a longer anesthesia duration, which itself increases postoperative pulmonary and cardiovascular risk. Similarly, persistent inflammation driven by adipokines, such as TNF-α and IL-6, along with chronically elevated hsCRP, contributes to impaired neutrophil function and increased susceptibility to infection. In patients with MetS, this immune dysregulation is further amplified by insulin resistance, which disrupts leukocyte chemotaxis and phagocytic capacity.
Another critical consideration is the diminished vascular reactivity associated with PVAT dysfunction. In the intraoperative setting, impaired perfusion increases the risk of anastomotic leaks and tissue necrosis, particularly in gastrointestinal procedures. Postoperatively, reduced vascular tone contributes to poor delivery of systemic antibiotics and nutrients essential for wound healing, prolonging recovery and increasing hospital length of stay. When examined alongside elevated PAI-1 levels and hypofibrinolysis, these findings provide a clear mechanistic explanation for why surgical patients with obesity and MetS experience more complications.
Perioperative optimization programs, such as Enhanced Recovery After Surgery (ERAS), are promising, as they improve outcomes by reducing surgical stress, enhancing mobilization, and standardizing postoperative care. However, in Puerto Rico, the successful integration of these evidence-based measures may require addressing infrastructural, economic, and access-related challenges. For example, nutrition counseling, prehabilitation programs, and structured weight-management interventions are not equally accessible across regions, potentially widening disparities in surgical fitness.
Despite these challenges, targeted approaches such as personalized risk assessment, preoperative metabolic optimization, and the selective use of minimally invasive techniques can significantly improve outcomes. As the population of Puerto Rico continues to age and obesity rates remain high, strengthening perioperative protocols tailored to patients with MetS will be essential for reducing the burden of surgical complications.
Conclusion
Obesity and Metabolic Syndrome are highly prevalent in Puerto Rico and represent major determinants of surgical risk. Their combined effects, including chronic inflammation, microvascular dysfunction, coagulation abnormalities, and impaired immune response, create a physiological environment that compromises wound healing and increases susceptibility to postoperative complications. In a population where nearly four out of five adults in the San Juan Metropolitan Area are overweight or obese, the impact on surgical practice is significant.
Addressing these challenges requires a comprehensive approach that integrates preventative public health strategies with perioperative optimization protocols. Implementing structured risk stratification, enhancing access to metabolic and nutritional interventions, and promoting minimally invasive surgical techniques are crucial steps toward improving outcomes. As Puerto Rico’s healthcare system navigates the rising burden of obesity-related disease, shaping surgical care to the metabolic realities of the population will play a fundamental role in reducing morbidity and advancing health equity.
References
- Pérez, C. M., Guzmán, M., Ortiz, A. P., Estrella, M., & Valle, Y. (2013). Prevalence of overweight and obesity and their cardiometabolic comorbidities in Puerto Rico. Puerto Rico Health Sciences Journal, 32(3), 122–129.
- National Heart, Lung, and Blood Institute. (2022). Clinical guidelines for metabolic syndrome. U.S. Department of Health and Human Services.
- Wilson, P. W. F., D’Agostino, R. B., Parise, H., Sullivan, L., & Meigs, J. B. (2005). Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation, 112(20), 3066–3072. https://doi.org/10.1161/CIRCULATIONAHA.105.539528
- Pinchuk, L., Smith, R. J., Martínez, A., & Lee, K. H. (2024). The role of hsCRP in chronic inflammatory states and impaired healing. Wound Repair and Regeneration, 32(1), 45–56. https://doi.org/10.1002/wrr.3501
- Khaled, S., & El-Din, A. (2024). Chronic inflammation and impaired wound healing in metabolic disorders. Journal of Inflammation Research, 17, 115–130.
- Fantuzzi, G. (2005). Adipose tissue, adipokines, and inflammation. Journal of Allergy and Clinical Immunology, 115(5), 911–919. https://doi.org/10.1016/j.jaci.2005.02.023 Kearney, J., Parsons, M. S., Donnelly, R., & Fisher, K. (2021). Fibrinogen and PAI-1 in metabolic syndrome: Pathophysiology and clinical relevance. Thrombosis Research, 198, 1–7. https://doi.org/10.1016/j.thromres.2020.10.020
- Sleiman, M., Clark, J. M., Patel, H., & Younes, N. (2021). Coagulation abnormalities in obesity and metabolic syndrome. Obesity Reviews, 22(6), e13245. https://doi.org/10.1111/obr.13245
- Aoqui, C., Chiazza, F., Patel, N. S., & Collino, M. (2014). Perivascular adipose tissue dysfunction and its contribution to vascular disease. Current Opinion in Pharmacology, 18, 121–127.
- Ri, M., Aikou, S., Seto, Y., Kumai, Y., Muraoka, A., & Mori, K. (2018). Impact of obesity on surgical outcomes in gastrointestinal surgery. Annals of Gastroenterological Surgery, 3(5), 475–484. https://doi.org/10.1002/ags3.12253
- Echahidi, N., Pibarot, P., Després, J.-P., Daigle, J.-M., Mohty, D., Cartier, R., Arsenault, M., Poirier, P., & Mathieu, P. (2007). Metabolic syndrome increases operative mortality in patients undergoing coronary artery bypass grafting surgery. Journal of the American College of Cardiology, 50(9), 843–851. https://doi.org/10.1016/j.jacc.2007.04.066
- Plassmeier, L. J., Schneider, R., Müller, K., & Bruckner, T. (2021). Enhanced Recovery After Surgery (ERAS) pathways in abdominal surgery: Outcomes and challenges. Annals of Surgery, 274(4), 650–658. https://doi.org/10.1097/SLA.0000000000005008
