Background
The Mental Health Parity and Addiction Equity Act (MHPAEA), passed in 2008 by Congress, is considered a major victory for access to mental health and substance use disorder treatment (MH/SUD). The law requires commercial health plans to provide mental health and substance use treatment “no more restrictive” than coverage for all other physical health/medical/surgical services. This law applies to state and local government insurance plans, private insurance sponsored plans, and those with individual market coverage.1,2 An important note is that MHPAE does not apply to Medicare, but a separate Medicare Improvements for Patients and Providers Act of 2008 did lower outpatient MH costs to meet medical treatment costs. 3
However, research dictates over the last decade since the law’s full implementation, there has been minimal effect on increasing access to treatment and decreasing the cost of care. This can be explained by lack of compliance by insurance companies and lack of regulation/enforcement from government agencies. States have varying levels of enforcement, which creates gaps and inequities in coverage across the United States. In a report to Congress in 2022, it was found commercial insurances were imposing coverage limits for years on behavioral health care without review. 3
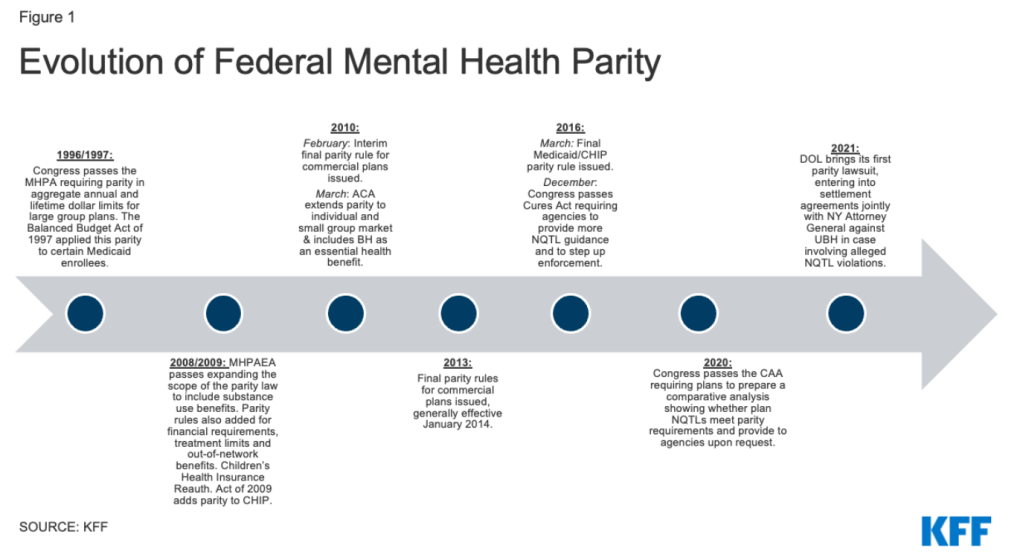
The evolution of mental health parity in the United States over the last 25 years. Image Provided by KFF. 3
What is affecting the enforcement of this law?
A recent case-study analyzed the implementation and effects of the MHPAEA on four states across the US and highlighted three distinct areas that are affecting how this law is enforced. These areas include:
- Relationships between the insurance commissioner (leader of insurance laws in a particular state) with other states/advocacy groups/insurance providers.
- Complexity of the law
- “Policy champions”: influential policy makers across the state who prioritize mental health equity and access.
Strong relationships among insurance leadership in the state/ federal government with other government entities and insurance stakeholders allows for information sharing, increased communication and problem solving.
A concern about the law’s language is that parts are vague and unclear in application, therefore there are challenges in understanding if insurers are complying. Additionally, there is a lack of public knowledge on this parity law, therefore people lack the knowledge of what may constitute a violation in one’s insurance or what should be covered.
Lastly, policy champions are necessary to enact change and movement with parity enforcement. Those in power that use their legislative position to make mental health/substance use treatment a priority issue sees greater funding allocation, more resources dedicated to the cause, and better enforcement. 1
Conclusions
The Mental Health Parity Act has been a major steppingstone for mental health and substance use treatment in the US, with the number of private insurance claims for behavioral health services has increasing 108% from 2007 to 2017, proof that “more people are getting treatment”. 4 However, there are still significant areas for improvement regarding enforcement and regulation. There are areas that could directly benefit the implementation of this law with increased attention and prioritization by lawmakers, simplifying standards and requirements, addressing physician/provider shortages, and increased enforcement tools to hold agencies accountable.
References
- Presskreischer, R., Barry, C. L., Lawrence, A. K., McCourt, A., Mojtabai, R., & McGinty, E. E. (2023). Factors Affecting State-Level Enforcement of the Federal Mental Health Parity and Addiction Equity Act: A Cross-Case Analysis of Four States. Journal of health politics, policy and law, 48(1), 1–34. https://doi.org/10.1215/03616878-10171062
- Presskreischer, R., Barry, C. L., Lawrence, A. K., McCourt, A., Mojtabai, R., & McGinty, E. E. (2023). Enforcement of the Mental Health Parity and Addiction Equity Act: State Insurance Commissioners’ Statutory Capacity. Psychiatric services (Washington, D.C.), 74(6), 652–655. https://doi.org/10.1176/appi.ps.20220210
- https://www.kff.org/mental-health/issue-brief/mental-health-parity-at-a-crossroads/
- https://www.managedhealthcareexecutive.com/view/parity-for-mental-health-any-progress-

